- The Stress in America™ survey measures attitudes and perceptions of stress among the general public.
March 20, 2024
By APA
Washington, DC – (Highpoint Digest) – U.S. society appears to be experiencing the psychological impacts of a collective trauma in the aftermath of the COVID-19 pandemic, according to the results of a new 2023 survey conducted by the American Psychological Association. Psychologists warn that a superficial characterization of life being “back to normal” is obscuring the post-traumatic effects on mental and physical health.
The long-term stress sustained since the COVID-19 pandemic began has had a significant impact on well-being, evidenced by a significant increase in reported mental health conditions and chronic illnesses, according to the results of Stress in America™ 2023, a nationwide survey conducted by The Harris Poll on behalf of APA among more than 3,000 U.S. adults age 18+.
The survey revealed that those ages 35 to 44 reported the most significant increase in chronic health conditions since the pandemic—58% in 2023 compared with 48% in 2019. Adults ages 35 to 44 also experienced the highest increase in mental health diagnoses—45% reported a mental illness in 2023 compared with 31% in 2019—though adults ages 18 to 34 still reported the highest rate of mental illnesses at 50% in 2023. Adults ages 35 to 44 were more likely to report that money (77% vs. 65%) and the economy (74% vs. 51%) were the factors that cause them significant stress today compared with 2019.
“The COVID-19 pandemic created a collective experience among Americans. While the early pandemic lockdowns may seem like the distant past, the aftermath remains,” said Arthur C. Evans Jr., PhD, APA’s chief executive officer. “We cannot ignore the fact that we have been significantly changed by the loss of more than one million Americans, as well as the shift in our workplaces, school systems and culture at large. To move toward post-traumatic growth, we must first identify and understand the psychological wounds that remain.”
APA psychologists noted that many people had generally positive perceptions of their physical health even when they reported being diagnosed with a chronic condition. More than four in five adults rated their physical health as good, very good, or excellent (81%), yet 66% of adults said they have been told by a healthcare provider that they have a chronic illness.
Furthermore, 81% of adults reported their mental health as good, very good or excellent, while more than one-third (37%) said they have a diagnosed mental health condition—a 5 percentage point increase from pre-pandemic levels in 2019 (32%).
Most adults also downplayed their stress; 67% said their problems aren’t “bad enough” to be stressed about, knowing that others have it worse. When asked why they don’t seek treatment, adults’ top reasons were the belief that therapy doesn’t work (40%), lack of time (39%) or lack of insurance (37%). Despite these reasons, nearly half (47%) said they wish they had someone to help manage their stress, and 62% reported they don’t talk about their stress because they don’t want to burden others.
Nearly a quarter of adults (24%) rated their average stress between eight and 10 on a scale of one to 10 where one means little to no stress and 10 means a great deal of stress. This is up from 19% in 2019, before the pandemic. This increase was mirrored across all age groups except those age 65+: 34% of those ages 18 to 34 reported this in 2023 (+8 percentage points from 2019); 31% of those 35 to 44 (+10 percentage points); 22% of those 45 to 64 (+4 percentage points); and 9% of those 65+ (-1 percentage point). Parents of children under the age of 18 who ranked their average stress between eight and 10 also saw a significant increase (33% in 2023 vs. 24% in 2019).
In 2023, parents were more likely than other adults to report that financial strain increased in their household (46% vs. 34%), that money is a cause of fights in their family (58% vs. 30%), and that they are more likely to feel consumed by worries regarding money (66% vs. 39%). Most troubling is that compared with other adults, parents of children under the age of 18 were more likely to report that on most days their stress is completely overwhelming (48% vs. 26%), they are so stressed they feel numb (42% vs. 22%) or on most days they are so stressed they can’t function (41% vs. 20%).
“Stress affects all systems of the body, so it is crucial that Americans know the serious impacts of stress and what they can do to reduce the effect of stressors in their life, as well as receive help from their health care providers, workplace and support systems to prevent further health crises,” said Evans.
A nation recovering from collective trauma
- The COVID-19 pandemic, global conflicts, racism and racial injustice, inflation, and climate-related disasters are all weighing on the collective consciousness of Americans
The national public health emergency around COVID-19 officially ended on May 11, 2023, and while the return to “normal” has been celebrated by many, results from the most recent Stress in America™ survey paint a different picture. Psychologists with APA say a superficial characterization of day-to-day life being more normal is obscuring the posttraumatic effects that have altered our mental and physical health.
When reviewing this year’s survey data, APA psychologists widely agreed there is mounting evidence that our society is experiencing the psychological impacts of a collective trauma.
“The COVID-19 pandemic created a collective experience among Americans. While the early-pandemic lockdowns may seem like the distant past, the aftermath remains,” said Arthur C. Evans Jr., PhD, APA’s chief executive officer.
Further, widespread trauma has not been limited to the pandemic. Global conflict, racism and racial injustice, inflation, and climate-related disasters are all weighing on the collective consciousness of Americans.
Stress in America 2023: A Nation Recovering from Collective Trauma examines the lasting psychological impacts of this combination of era-defining crises. An inspection of pre- and post-pandemic mental and physical health reveals signs of collective trauma among all age cohorts.
The data suggested the long-term stress sustained since the COVID-19 pandemic began had a significant impact on well-being, evidenced by an increase in chronic illnesses—especially among those between the ages of 35 and 44, which increased from 48% reported in 2019 to 58% in 2023. Adults ages 35 to 44 also experienced the highest increase in mental health diagnoses—from 31% reported in 2019 to 45% in 2023—though adults ages 18 to 34 still reported the highest rate of mental illnesses at 50% in 2023.
on the other hand, Psychological science has revealed that long-term stress creates risks for a variety of mental health challenges, may make us feel more sensitive even to daily hassles, can have broader impacts on our general life outlook and goals, and affects the body’s physiological response to stressors in ways that have notable implications for our physical health. Coping with long-term stress requires a different set of skills than adjusting to temporary stressors.
Stress often puts the body on high alert and ongoing stress can accumulate, causing inflammation, wearing on the immune system, and increasing the risk of a host of ailments, including digestive issues, heart disease, weight gain, and stroke.
“We cannot ignore the fact that we have been significantly changed by the loss of more than one million Americans, as well as the shift in our workplaces, school systems, and culture at large. To move toward posttraumatic growth, we must first identify and understand the psychological wounds that remain,” said Evans.
The effects of Stress on the body
Our bodies are well equipped to handle stress in small doses, but when that stress becomes long-term or chronic, it can have serious effects on your body.
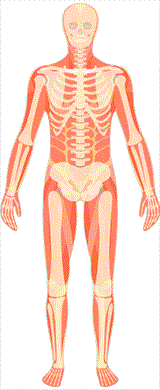
Musculoskeletal system
When the body is stressed, muscles tense up. Muscle tension is almost a reflex reaction to stress—the body’s way of guarding against injury and pain.
With sudden onset stress, the muscles tense up all at once, and then release their tension when the stress passes. Chronic stress causes the muscles in the body to be in a more or less constant state of guardedness. When muscles are taut and tense for long periods of time, this may trigger other reactions of the body and even promote stress-related disorders.
For example, both tension-type headache and migraine headache are associated with chronic muscle tension in the area of the shoulders, neck and head. Musculoskeletal pain in the low back and upper extremities has also been linked to stress, especially job stress.
Millions of individuals suffer from chronic painful conditions secondary to musculoskeletal disorders. Often, but not always, there may be an injury that sets off the chronic painful state. What determines whether or not an injured person goes on to suffer from chronic pain is how they respond to the injury. Individuals who are fearful of pain and re-injury, and who seek only a physical cause and cure for the injury, generally have a worse recovery than individuals who maintain a certain level of moderate, physician-supervised activity. Muscle tension, and eventually, muscle atrophy due to disuse of the body, all promote chronic, stress-related musculoskeletal conditions.
Relaxation techniques and other stress-relieving activities and therapies have been shown to effectively reduce muscle tension, decrease the incidence of certain stress-related disorders, such as headache, and increase a sense of well-being. For those who develop chronic pain conditions, stress-relieving activities have been shown to improve mood and daily function.
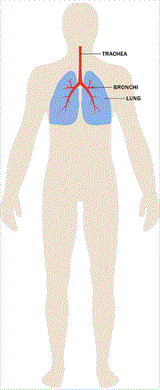
Respiratory system
The respiratory system supplies oxygen to cells and removes carbon dioxide waste from the body. Air comes in through the nose and goes through the larynx in the throat, down through the trachea, and into the lungs through the bronchi. The bronchioles then transfer oxygen to red blood cells for circulation.
Stress and strong emotions can present with respiratory symptoms, such as shortness of breath and rapid breathing, as the airway between the nose and the lungs constricts. For people without respiratory disease, this is generally not a problem as the body can manage the additional work to breathe comfortably, but psychological stressors can exacerbate breathing problems for people with pre-existing respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD; includes emphysema and chronic bronchitis).
Some studies show that an acute stress—such as the death of a loved one—can actually trigger asthma attacks. In addition, the rapid breathing—or hyperventilation—caused by stress can bring on a panic attack in someone prone to panic attacks.
Working with a psychologist to develop relaxation, breathing, and other cognitive behavioral strategies can help.
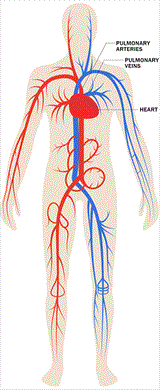
Cardiovascular system
The heart and blood vessels comprise the two elements of the cardiovascular system that work together in providing nourishment and oxygen to the organs of the body. The activity of these two elements is also coordinated in the body’s response to stress. Acute stress—stress that is momentary or short-term such as meeting deadlines, being stuck in traffic or suddenly slamming on the brakes to avoid an accident—causes an increase in heart rate and stronger contractions of the heart muscle, with the stress hormones—adrenaline, noradrenaline, and cortisol—acting as messengers for these effects.
In addition, the blood vessels that direct blood to the large muscles and the heart dilate, thereby increasing the amount of blood pumped to these parts of the body and elevating blood pressure. This is also known as the fight or flight response. Once the acute stress episode has passed, the body returns to its normal state.
Chronic stress, or a constant stress experienced over a prolonged period of time, can contribute to long-term problems for heart and blood vessels. The consistent and ongoing increase in heart rate, and the elevated levels of stress hormones and of blood pressure, can take a toll on the body. This long-term ongoing stress can increase the risk for hypertension, heart attack, or stroke.
Repeated acute stress and persistent chronic stress may also contribute to inflammation in the circulatory system, particularly in the coronary arteries, and this is one pathway that is thought to tie stress to heart attack. It also appears that how a person responds to stress can affect cholesterol levels.
The risk for heart disease associated with stress appears to differ for women, depending on whether the woman is premenopausal or postmenopausal. Levels of estrogen in premenopausal women appears to help blood vessels respond better during stress, thereby helping their bodies to better handle stress and protecting them against heart disease. Postmenopausal women lose this level of protection due to loss of estrogen, therefore putting them at greater risk for the effects of stress on heart disease.

Endocrine system
When someone perceives a situation to be challenging, threatening, or uncontrollable, the brain initiates a cascade of events involving the hypothalamic-pituitary-adrenal (HPA) axis, which is the primary driver of the endocrine stress response. This ultimately results in an increase in the production of steroid hormones called glucocorticoids, which include cortisol, often referred to as the “stress hormone”.
The HPA axis
During times of stress, the hypothalamus, a collection of nuclei that connects the brain and the endocrine system, signals the pituitary gland to produce a hormone, which in turn signals the adrenal glands, located above the kidneys, to increase the production of cortisol.
Cortisol increases the level of energy fuel available by mobilizing glucose and fatty acids from the liver. Cortisol is normally produced in varying levels throughout the day, typically increasing in concentration upon awakening and slowly declining throughout the day, providing a daily cycle of energy.
During a stressful event, an increase in cortisol can provide the energy required to deal with prolonged or extreme challenge.
Stress and health
Glucocorticoids, including cortisol, are important for regulating the immune system and reducing inflammation. While this is valuable during stressful or threatening situations where injury might result in increased immune system activation, chronic stress can result in impaired communication between the immune system and the HPA axis.
This impaired communication has been linked to the future development of numerous physical and mental health conditions, including chronic fatigue, metabolic disorders (e.g., diabetes, obesity), depression, and immune disorders.

Gastrointestinal system
The gut has hundreds of millions of neurons which can function fairly independently and are in constant communication with the brain—explaining the ability to feel “butterflies” in the stomach. Stress can affect this brain-gut communication, and may trigger pain, bloating, and other gut discomfort to be felt more easily. The gut is also inhabited by millions of bacteria which can influence its health and the brain’s health, which can impact the ability to think and affect emotions.
Stress is associated with changes in gut bacteria which in turn can influence mood. Thus, the gut’s nerves and bacteria strongly influence the brain and vice versa.
Early life stress can change the development of the nervous system as well as how the body reacts to stress. These changes can increase the risk for later gut diseases or dysfunctioning.
Esophagus
When stressed, individuals may eat much more or much less than usual. More or different foods, or an increase in the use of alcohol or tobacco, can result in heartburn or acid reflux. Stress or exhaustion can also increase the severity of regularly occurring heartburn pain. A rare case of spasms in the esophagus can be set off by intense stress and can be easily mistaken for a heart attack.
Stress also may make swallowing foods difficult or increase the amount of air that is swallowed, which increases burping, gassiness, and bloating.
Stomach
Stress may make pain, bloating, nausea, and other stomach discomfort felt more easily. Vomiting may occur if the stress is severe enough. Furthermore, stress may cause an unnecessary increase or decrease in appetite. Unhealthy diets may in turn deteriorate one’s mood.
Contrary to popular belief, stress does not increase acid production in the stomach, nor causes stomach ulcers. The latter are actually caused by a bacterial infection. When stressed, ulcers may be more bothersome.
Bowel
Stress can also make pain, bloating, or discomfort felt more easily in the bowels. It can affect how quickly food moves through the body, which can cause either diarrhea or constipation. Furthermore, stress can induce muscle spasms in the bowel, which can be painful.
Stress can affect digestion and what nutrients the intestines absorb. Gas production related to nutrient absorption may increase.
The intestines have a tight barrier to protect the body from (most) food related bacteria. Stress can make the intestinal barrier weaker and allow gut bacteria to enter the body. Although most of these bacteria are easily taken care of by the immune system and do not make us sick, the constant low need for inflammatory action can lead to chronic mild symptoms.
Stress especially affects people with chronic bowel disorders, such as inflammatory bowel disease or irritable bowel syndrome. This may be due to the gut nerves being more sensitive, changes in gut microbiota, changes in how quickly food moves through the gut, and/or changes in gut immune responses.
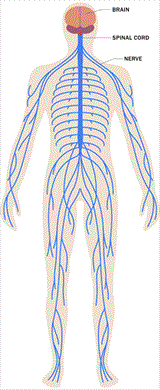
Nervous system
The nervous system has several divisions: the central division involving the brain and spinal cord and the peripheral division consisting of the autonomic and somatic nervous systems.
The autonomic nervous system has a direct role in physical response to stress and is divided into the sympathetic nervous system (SNS), and the parasympathetic nervous system (PNS). When the body is stressed, the SNS contributes to what is known as the “fight or flight” response. The body shifts its energy resources toward fighting off a life threat, or fleeing from an enemy.
The SNS signals the adrenal glands to release hormones called adrenalin (epinephrine) and cortisol. These hormones, together with direct actions of autonomic nerves, cause the heart to beat faster, respiration rate to increase, blood vessels in the arms and legs to dilate, digestive process to change and glucose levels (sugar energy) in the bloodstream to increase to deal with the emergency.
The SNS response is fairly sudden in order to prepare the body to respond to an emergency situation or acute stress—short term stressors. Once the crisis is over, the body usually returns to the pre-emergency, unstressed state. This recovery is facilitated by the PNS, which generally has opposing effects to the SNS. But PNS over-activity can also contribute to stress reactions, for example, by promoting bronchoconstriction (e.g., in asthma) or exaggerated vasodilation and compromised blood circulation.
Both the SNS and the PNS have powerful interactions with the immune system, which can also modulate stress reactions. The central nervous system is particularly important in triggering stress responses, as it regulates the autonomic nervous system and plays a central role in interpreting contexts as potentially threatening.
Chronic stress, experiencing stressors over a prolonged period of time, can result in a long-term drain on the body. As the autonomic nervous system continues to trigger physical reactions, it causes a wear-and-tear on the body. It’s not so much what chronic stress does to the nervous system, but what continuous activation of the nervous system does to other bodily systems that become problematic.
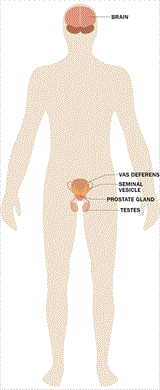
Male reproductive system
The male reproductive system is influenced by the nervous system. The parasympathetic part of the nervous system causes relaxation whereas the sympathetic part causes arousal. In the male anatomy, the autonomic nervous system, also known as the fight or flight response, produces testosterone and activates the sympathetic nervous system which creates arousal.
Stress causes the body to release the hormone cortisol, which is produced by the adrenal glands. Cortisol is important to blood pressure regulation and the normal functioning of several body systems including cardiovascular, circulatory, and male reproduction. Excess amounts of cortisol can affect the normal biochemical functioning of the male reproductive system.
Sexual desire
Chronic stress, ongoing stress over an extended period of time, can affect testosterone production resulting in a decline in sex drive or libido, and can even cause erectile dysfunction or impotence.
Reproduction
Chronic stress can also negatively impact sperm production and maturation, causing difficulties in couples who are trying to conceive. Researchers have found that men who experienced two or more stressful life events in the past year had a lower percentage of sperm motility (ability to swim) and a lower percentage of sperm of normal morphology (size and shape), compared with men who did not experience any stressful life events.
Diseases of the reproductive system
When stress affects the immune system, the body can become vulnerable to infection. In the male anatomy, infections to the testes, prostate gland, and urethra, can affect normal male reproductive functioning.
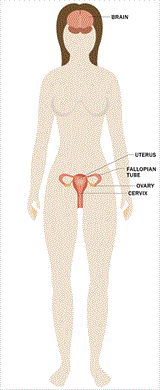
Female reproductive system
Menstruation
Stress may affect menstruation among adolescent girls and women in several ways. For example, high levels of stress may be associated with absent or irregular menstrual cycles, more painful periods, and changes in the length of cycles.
Sexual desire
Women juggle personal, family, professional, financial, and a broad range of other demands across their life span. Stress, distraction, fatigue, etc., may reduce sexual desire—especially when women are simultaneously caring for young children or other ill family members, coping with chronic medical problems, feeling depressed, experiencing relationship difficulties or abuse, dealing with work problems, etc.
Pregnancy
Stress can have significant impact on a woman’s reproductive plans. Stress can negatively impact a woman’s ability to conceive, the health of her pregnancy, and her postpartum adjustment. Depression is the leading complication of pregnancy and postpartum adjustment.
Excess stress increases the likelihood of developing depression and anxiety during this time. Maternal stress can negatively impact fetal and ongoing childhood development and disrupt bonding with the baby in the weeks and months following delivery.
Premenstrual syndrome
Stress may make premenstrual symptoms worse or more difficult to cope with and premenses symptoms may be stressful for many women. These symptoms include cramping, fluid retention and bloating, negative mood (feeling irritable and “blue”) and mood swings.
Menopause
As menopause approaches, hormone levels fluctuate rapidly. These changes are associated with anxiety, mood swings, and feelings of distress. Thus menopause can be a stressor in and of itself. Some of the physical changes associated with menopause, especially hot flashes, can be difficult to cope with.
Furthermore, emotional distress may cause the physical symptoms to be worse. For example, women who are more anxious may experience an increased number of hot flashes and/or more severe or intense hot flashes.
Diseases of the reproductive system
When stress is high, there is increased chance of exacerbation of symptoms of reproductive disease states, such as herpes simplex virus or polycystic ovarian syndrome. The diagnosis and treatment of reproductive cancers can cause significant stress, which warrants additional attention and support.
Stress management
These recent discoveries about the effects of stress on health shouldn’t leave you worrying. We now understand much more about effective strategies for reducing stress responses. Such beneficial strategies include:
- Maintaining a healthy social support network
- Engaging in regular physical exercise
- Getting an adequate amount of sleep each night
These approaches have important benefits for physical and mental health, and form critical building blocks for a healthy lifestyle. If you would like additional support or if you are experiencing extreme or chronic stress, a licensed psychologist can help you identify the challenges and stressors that affect your daily life and find ways to help you best cope for improving your overall physical and mental well-being.
APA gratefully acknowledges the assistance of William Shaw, PhD; Susan Labott-Smith, PhD, ABPP; Matthew M. Burg, PhD; Camelia Hostinar, PhD; Nicholas Alen, BA; Miranda A.L. van Tilburg, PhD; Gary G. Berntson, PhD; Steven M. Tovian, PhD, ABPP, FAClinP, FAClinHP; and Malina Spirito, PsyD, MEd; in developing this article.
Source: American Psychological Association
Images courtesy of American Psychological Association